The five countries that make up Central Asia—Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan and Uzbekistan—have a total population of more than 60 million and considerable ethnic, cultural, and religious diversity. In 2019, the region celebrated the thirtieth anniversary of HIV services, which were established in 1989 in the Republics of the former Soviet Union. The current HIV epidemics and national HIV control programmes in Central Asian countries share many similarities, although there are also differences. Given the lack of reliable data on people living with HIV in Turkmenistan and Uzbekistan, this article will focus on Kazakhstan, Kyrgyzstan and Tajikistan.
By signing the 2016 United Nations Political Declaration on ending AIDS,1 Kazakhstan, Kyrgyzstan and Tajikistan have declared their commitment to accelerate efforts towards ending the AIDS epidemic by 2030, which implies reaching three key goals. The first is ensuring that people living with HIV live long and healthy lives, which means that all of them would know their HIV status, receive antiretroviral therapy (ART) and have undetectable levels of viremia (suppressed viral load). The second goal is to reduce the number of new HIV infections; the third—to eliminate HIV-related stigma and discrimination. In addition, the mayors of three large cities—Almaty in Kazakhstan, and Bishkek and Osh in Kyrgyzstan—have committed to putting cities on the fast-track to ending the HIV epidemic.
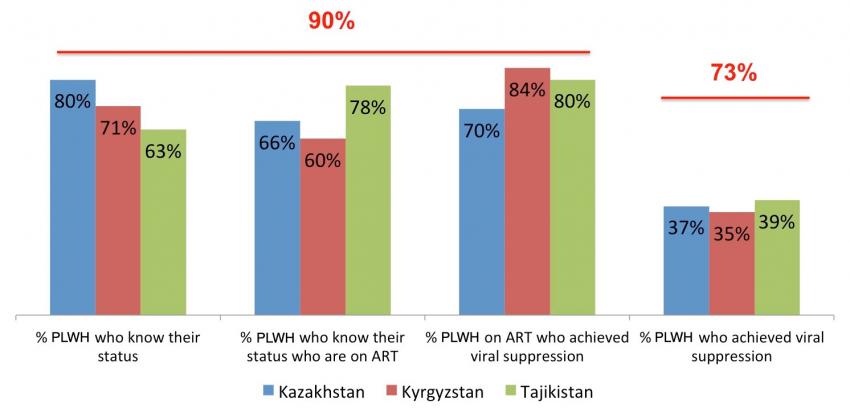
The most recent UNAIDS estimates show that in 2018 there were 26,000 people living with HIV in Kazakhstan, 8,500 in Kyrgyzstan, and 13,000 in Tajikistan.2 In recent years, all three countries have made substantial progress in ensuring that more people are tested for HIV and begin ART. Nonetheless, according to the nationally reported data, as of October 2019, the proportion of estimated PLWH with suppressed viremia in the region remains well below the desired target of 73 per cent needed to turn the curve of the HIV epidemic (Graph 1, below).
There are many factors that continue to fuel and facilitate HIV epidemics and hinder effective responses. Therefore, despite the progress and commitments, reaching effective epidemic control is unlikely to be achieved by 2020 in Central Asia.
Injecting drug use. Central Asia is located on the trafficking route from Afghanistan to Europe, which makes opioids relatively accessible and leads to high rates of use. The increasing number of people injecting synthetic cathinones (“bath salts”) and other non-opioid drugs poses an additional challenge to HIV prevention efforts. By the end of 2018, national HIV programme data showed that approximately 40 per cent of all people living with HIV in Kazakhstan and Kyrgyzstan, and 30 per cent in Tajikistan, reported a history of injecting drug use or were currently injecting drugs.3 Sex partners of people who inject drugs (PWID) also accounted for a significant proportion of all sexually transmitted HIV infections. An excessive emphasis on punitive measures has been an inherent feature of drug control and addiction treatment in countries in Central Asia. The broadly accepted registration of all people with addiction disorders leads to the restriction of their civil rights, including employability, and to reluctance among PWID to engage with health services. The criminalization of drug use has also led to high rates of incarceration. Limited access to comprehensive harm reduction options during incarceration, lack of effective adherence support for incarcerated people living with HIV, and limited continuation of care for people living with HIV transition to or from penitentiaries also contribute to the spread of HIV.
It is widely acknowledged that needle and syringe programmes and opioid agonist therapy (OAT) decrease HIV incidence among PWID. OAT also supports the adherence of people living with HIV to ART. Options for quality pharmacological treatment of substance dependence, rehabilitation, recovery and social reintegration are limited. Access to methadone-based OAT remains alarmingly low in the region, with less than 5 per cent of the estimated number of PWID benefiting from existing programmes.4 To expand access to treatment, countries are planning to pilot buprenorphine-based OAT. Other forms of maintenance therapy, such as those based on extended-release naltrexone, morphine and medical-grade heroin, have not yet even been discussed.
High mobility. Kazakhstan borders Russia, which accounts for the majority of newly diagnosed HIV infections in Europe. It is also a top destination for migrant workers from throughout Central Asia. In fact, over the past several years, mobility has become an important HIV risk factor, with 17.3 per cent of all people newly diagnosed with HIV in Tajikistan in 2018 reporting a recent history of migration and no history of injecting drug use. Programs to ensure cross-country HIV prevention and treatment interventions for migrant populations are limited to a few fragmented pilot projects, leaving most people living with HIV without access to ART while in migration.
Stigma and discrimination. HIV-related stigma and discrimination against people living with HIV by law enforcement, health-care workers and members of their own communities continue to stand as barriers to effective HIV epidemic control. Tradition-oriented customs, religious beliefs and gender norms that discourage discussion about sexual behaviour, even among adults, hinder successful HIV prevention and targeted testing efforts. The global HIV epidemic has always been linked to men who have sex with men, but HIV among men who have sex with men in the region is understudied. Transgender people and men who have sex with men face strong social pressure and stigma, with frequent reports of violence against community members, which also limits access to services.
Service delivery and programmatic challenges. Due to funding restrictions and rigid bureaucratic regulations related to health service provision, countries in Central Asia have been relatively slow to adopt innovative and progressive approaches to HIV prevention and treatment programming. HIV testing is mostly provider-initiated, with only limited community-based and self-testing options available. HIV testing algorithms are complex, and confirmation of diagnosis can take considerable time. The transition to newer, more effective dolutegravir-based treatment regimens has been slow, and many people take multi-tablet regimens that are less tolerated and have higher susceptibility to drug resistance. Pre-exposure prophylaxis (PrEP), an effective method for preventing HIV acquisition among individuals at high risk, has not yet been rolled out widely in Central Asia.

Conclusion. To achieve HIV epidemic control, countries in Central Asia will need to address fundamental factors that drive HIV transmission and impede the engagement of people living with HIV and key populations, such as substance users, transgender and gay people, and other men who have sex with men, in effective prevention and treatment programmes. This includes zero tolerance for HIV-related stigma and discrimination, and intensive advocacy to overcome deep societal prejudices towards key populations, as well as concerted efforts to shape HIV responses to unique needs. Epidemic control will also require decriminalization of drug use and ending the requirement for and the practice of registration of persons with substance use disorders. HIV programming needs to shift from a top-down approach to more active and meaningful community engagement. Prevention of new HIV infections will require expanding access to key evidence-based primary prevention interventions, such as harm reduction and medication-assisted maintenance programmes for PWID. In addition, the adoption of innovations is urgently needed, including the expansion of self-testing options, PrEP and community-based distribution. With the decrease in external HIV funding for Central Asian countries, it also becomes crucially important to garner strong political will and ensure the optimization of national resources to enable the implementation of evidence-based interventions for HIV prevention, testing, linkage to treatment and adherence support.
The author acknowledges the support of Ms. Sarina Dane, Senior Project Officer at ICAP, Columbia University, in the development of this article.
Notes
1 Political Declaration on HIV and AIDS: On the Fast Track to Accelerating the Fight against HIV and to Ending the AIDS Epidemic by 2030 (A/RES/70/266). Available at https://documents-dds-ny.un.org/doc/UNDOC/GEN/N16/164/34/pdf/N1616434.pdf?OpenElement.
2 Data available from http://aidsinfo.unaids.org/
3 Anna P. Deryabina and Wafaa M. El-Sadr, “Optimizing HIV prevention and treatment outcomes for persons with substance use in Central Asia: what will it take?”, Current Opinion in HIV and AIDS, vol. 14, No. 5 (September 2019), p. 374. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6688715/.
4 Ibid.
The UN Chronicle is not an official record. It is privileged to host senior United Nations officials as well as distinguished contributors from outside the United Nations system whose views are not necessarily those of the United Nations. Similarly, the boundaries and names shown, and the designations used, in maps or articles do not necessarily imply endorsement or acceptance by the United Nations.




